Therapy poster - incontinence in aged care.pub
SUGGESTIONS TO IMPROVE THE HEALTH AND SAFETY OF RESIDENTS
TYPES OF INCONTINENCE
DIET AND TOILETING HABITS
Incontinence can either be urinary of faecal.
’éå’ĆĀThe bladder can hold between 1┬Į ŌĆō 2┬Į cups of urine (300-400mls). On average a person should wee about 5-
Urinary incontinence affects over a third of the total population and women > men at a
8x/day (over 24hrs) or roughly every 3-4 hrs (for larger bladders it may be every 4-8hrs). If an individual is
considerably outside these averages then more attention and further assessment may be needed.
Faecal incontinence affects roughly 3-9% of all elderly Australians, increasing to 10-30% in
Encourage adequate fluid intake spread evenly throughout the day (6-8 cups or 1.5-2L/day). This includes
cordial, juice, tea, coffee etc. but try to avoid too much caffeine or alcohol as it irritates the bladder.
Incontinence is an issue that significantly impacts upon one's physical, psychological and
’éå’ĆĀDiscourage going to the toilet 'just in case' (e.g. every time an individual gets up to leave the room or make a
social well-being. It becomes increasingly more common with age but does not have to be
cup of tea etc.) as this reduces how much the bladder is able to hold.
an inevitable consequence of growing older.
’éå’ĆĀDiscourage reducing fluid intake as this concentrates the urine, making the problem worse, not better.
’éå’ĆĀEncourage the individual to check they've fully emptied their bladder before getting off the toilet as
It is currently one of the top six reasons that influence a family's decision to seek
retention can lead to bladder dysfunction and UTI's.
residential care for their relative. However, this issue can be successfully addressed with
a good awareness of contributing factors, preventative methods and treatment options.
A healthy, varied diet is extremely beneficial. We need 30g of fibre on average to keep our bowels healthy. Much can be obtained from wholegrains, cereals, legumes, nuts, seeds, fresh fruit and vegetables, but a fibre supplement such as Metamucil, Benefibre, Fybogel or Normafibre (better for individuals with IBS) is a
CONTRIBUTING FACTORS
It's a good idea to try to recognise certain issues that can lead to incontinence and check that they are being managed correctly. These can be remembered with the acronym,
’éå’ĆĀDiscourage prolonged periods of time without eating (even just
D = Delirium
a piece of fruit or a biscuit every so often) as this helps to keep
I = Infection (e.g. UTI)
A = Atrophic urethritis or vaginitis (common with decreased oestrogen after menopause)
P = Psychological (e.g. depression, delirium, pain)
’éå’ĆĀGentle, daily mobility (as able) also greatly helps to stimulate
P = Pharmacological (e.g. certain anti-hypertensives, diuretics, analgesia)
E = Excess urine output
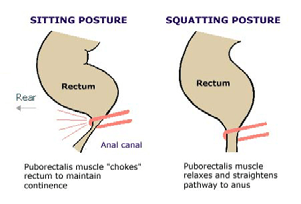
’éå’ĆĀWhen sitting on the toilet, it is much better to adopt a
R = Restricted mobility
squatting > sitting position as this helps the bowels to open
S = Stool impaction (constipation) or IBS
more naturally, as this picture (left) shows:
Other issues to be aware of include:
’éå’ĆĀdeclining cognitive function (e.g. dementia, Parkinsons)
’éå’ĆĀunstable diabetes (as this can increase fluid intake and output)
’éå’ĆĀPosition a footstool under the feet so that the knees are above the hips. Have the legs apart, the back
straight, the chest forwards, with arms leaning on legs (if able). Encourage the stomach and anal opening be
kept relaxed with steady even breathing.
PREVENTATIVE METHODS
There should be no straining or breath holding! Try to allow good amount of time for complete emptying. If
Promotion of good lifestyle habits can help to prevent incontinence. These include:
bowels aren't opening, encourage getting up, going for a walk or doing something else and coming back later.
’éå’ĆĀWeight management and avoidance of obesity
’éå’ĆĀEffective management of a chronic cough (e.g. due to smoking)
’é©’ĆĀ Overall, these techniques can help to reduce the need for methods that are harsher on the bowels, such as,
regular coloxyl and senna which can lead to bad cycles of constipation followed by incontinence and loose
’éå’ĆĀAppropriate hydration, diet and toileting habits
’éå’ĆĀMaintenance of functional activity and mobility
Treatment options
’éå’ĆĀCollect all equipment required/prepare the environment (move the bed away from Further management for incontinence issues can include:
necessary, ensure brakes are on, adjust the height of the bed so that the client's feet
’éå’ĆĀbladder/bowel retraining and pelvic floor exercises (by a trained physiotherapist)
can touch the floor, provide walking aid, etc)
’éå’ĆĀEnsure the client is positioned on their back on a folded slide sheet (folded side to ’éå’ĆĀcertain medications (e.g. anticholinergic agent, oxybutynin which increases bladder capacity)
edge of bed ŌĆō see bed mobility section of this manual), and position lower limbs so
’éå’ĆĀor sometimes even surgical intervention
Wellness & Lifestyles Australia finds significance in its work by using allied health therapists to service those less fortunate, but also to
educate others on how they can assist. For more information on this poster or to find out more about our services, please contact us!
Phone: (08) 8331 3000
Email: contact@wellnesslifestyles.com.au Website: www.wleducation.com.au
Source: http://www.wleducation.com.au/posters/incontinence-in-aged-care-poster.pdf
OFFICE OF CATHOLIC SCHOOLS DIOCESE OF ARLINGTON ASTHMA ACTION PLAN PROCEDURES ON REVERSE TO BE COMPLETED BY PARENT: Student ________________________________________ DOB _____________ School ___________________________________ Grade __________ Emergency Contact ________________________________________________ Relationship _______________________ Phone _____________
A Newsletter from Harvard Business School Publishing Will Project Creep Cost YouŌĆöor Create Value? by Loren Gary For reprint and subscription information For customized and quantity orders of reprints: Call 617-783-7626 Fax 617-783-7658 Call 800-988-0866 or 617-783-7500 Will Project Creep Cost YouŌĆöor Create Value? Strict rules that limit a projectŌĆ
A |
B |
C |
D |
E |
F |
G |
H |
I |
J |
K |
L |
M |
N |
O |
P |
Q |
R |
S |
T |
U |
V |
W |
X |
Y |
Z |
0-9 |






 SUGGESTIONS TO IMPROVE THE HEALTH AND SAFETY OF RESIDENTS
SUGGESTIONS TO IMPROVE THE HEALTH AND SAFETY OF RESIDENTS