Woundviewer.med-surv.de
JASN Express . Published on March 23, 2005 as doi: 10.1681/ASN.2004110997
Randomized, Controlled Trial of Topical Exit-Siteversus Mupirocin for the
David Wayne Johnson, Carolyn van Eps, David William Mudge, Kathryn Joan Wiggins,Kirsty Armstrong, Carmel Mary Hawley, Scott Bryan Campbell, Nicole Maree Isbel,Graeme Robert Nimmo, and Harry Gibbs
Department of Renal Medicine, University of Queensland at Princess Alexandra Hospital, Brisbane, Australia
The clinical usefulness of hemodialysis catheters is limited by increased infectious morbidity and mortality. Topical antisepticversus mupirocin in preventing catheter-associated infections. A randomized, controlled trial was performed comparingversus mupirocin on infection rates in patients who weren ЎН
51) and mupirocin-treated (n ЎН
50) patients were comparable (0.97 versus 0.85 episodes per 1000 catheter-days, respectively; NS). On Cox proportional hazards model analysis, the use of honey was notP ЎН
0.92). No exit-site infections occurred. During the study period, 2% of staphylococcal isolates within the hospital were
J Am Soc Nephrol 16: ???вАУ???, 2005. doi: 10.1681/ASN.2004110997
C entralvenouscatheterizationisanestablishedmethodof siteinfection,andbacteremiacomparedwithnontunneledand
providing rapid, temporary access for the provision of
noncuffed devices (9вАУ14). Recently, our group demonstrated that
hemodialysis to patients with serious acute or chronic
the topical application of 2% mupirocin ointment to the exit sites
renal failure. Unfortunately, the clinical usefulness of this method
of hemodialysis patients with tunneled, cuffed catheters engen-
is severely limited by the frequent occurrence of bloodstream
dered a further reduction in the rates of catheter-associated staph-
infections in up to 40% of cases (1вАУ3). A number of registry (4,5)
ylococcal exit-site infection and bacteremia (3). Median infection-
and observational cohort studies (6) have indicated that there has
free survival time was increased from 55 to 108 d, such that one
been an increasing reliance on hemodialysis catheters in incident
episode of bacteremia was prevented for every 3.7 patients
hemodialysis patients ranging from 30% of patients in Europe and
treated. Unfortunately, a potentially significant disadvantage of
Australia to 60% in the United States. Recent studies have sug-
mupirocin chemoprophylaxis is the appearance of resistant staph-
gested further that the use of hemodialysis catheters is associated
ylococcal strains, which have been reported in a number of units
with a 1.5- to 3-fold increase in both all-cause and infectious
in other hospitals (15). It would clearly be ideal to develop an
mortality (4,7,8). A number of randomized, controlled trials have
alternative, safer strategy to mupirocin for preventing catheter-
demonstrated convincingly that tunneled, cuffed catheters are
associated infections without selecting further resistant strains.
associated with a much lower risk for bacterial colonization, exit-
A promising agent in this regard is honey. Honey has been
used from ancient times as a method of accelerating woundhealing (16) and is mentioned for healing purposes in the Bible,
Received November 24, 2004. Accepted February 11, 2005.
the Koran, and the Torah (17). Anecdotally, honey has been
Published online ahead of print. Publication date available at www.jasn.org.
claimed to reduce inflammation; debride necrotic tissue; reduce
Address correspondence to: Prof. David Johnson, Department of Renal Medicine,
edema; and promote angiogenesis, granulation, and epithelial-
Level 2, Ambulatory Renal and Transplant Services Building, Princess Alexandra
ization (18). More recently, there have been a number of reports
Hospital, Ipswich Road, Woolloongabba, Brisbane, Queensland 4102, Australia.
of honey being used successfully as a dressing for wounds,
Phone: ѕ©61-7-3240-5080; Fax: ѕ©61-7-3240-5480; E-mail: david_johnson@health.
qld.gov.au
including burns, ulcers, infected surgical wounds, necrotizing
Copyright 2005 by the American Society of Nephrology
Journal of the American Society of Nephrology
soft tissue infections, meningococcal wounds, and abdominal
Central venous catheters were dedicated to hemodialysis use and were
wound dehiscence (17,19 вАУ21). A meta-analysis of seven ran-
not accessed for other purposes. Subsequent catheter-site care was
domized, controlled trials involving the use of honey as a
performed by trained hemodialysis registered nurses using a rigorous
wound dressing showed it to be superior to antiseptics and/or
aseptic technique. Primapore dressings were changed thrice weekly ateach hemodialysis treatment, and the sites were recleansed with 10%
systemic antibiotics for wound healing, maintenance of steril-
povidone iodine solution, in accordance with the Kidney Disease Out-
ity, and eradication of infection (22).
comes Quality Initiative guidelines (27). Patients who were allocated to
In laboratory studies, some honeys have been shown to exert
the honey group additionally received approximately 3 ml of Medi-
an antimicrobial action against a broad spectrum of fungi and
honey applied to their exit sites with each dressing change. Patients
bacteria, including antibiotic-resistant bacteria such as methi-
who were allocated to the mupirocin group had mupirocin ointment
cillin-resistant
Staphylococcus aureus , multidrug-resistant gram
applied to their exit sites with each dressing change according to
negative organisms, and vancomycin-resistant enterococci
standard unit protocols (approximately 10 mm of ointment was
(23,24). The reasons for this antibacterial activity include a
squeezed directly on to their exit sites from a 15-g tube with an outlet
relatively low water activity (0.56 to 0.59), low pH (3.2 to 4.5),
diameter of 5 mm with each dressing change). Patients were treated
the production of hydrogen peroxide on dilution (as a result of
with topical honey or mupirocin for the entire period that their catheter
the presence of the enzyme glucose oxidase), and phytochem-
remained
in situ . At the completion of each hemodialysis treatment,sodium heparin (1000 U/ml) was injected into each lumen in a volume
ical components (including flavonoids and phenolic acids) (24).
equivalent to the priming volume of the catheter.
Despite a considerable accumulated experience of honey use in
At the time of inclusion in the study, demographic and clinical data
wound infections, antimicrobial resistance has not yet been
were recorded. Patients had their anterior nares cultured for
S. aureus ,
reported, thereby making it very attractive as a potential means
but identified nasal carriers were not treated. Patients were followed up
of antimicrobial prophylaxis (25). The aim of the present study
until the catheter was removed. The primary outcome measure was
was to determine the efficacy and the safety of topical exit-site
catheter-related bacteremia. Secondary outcome measures included
application of standardized antibacterial honey (Medihoney)
catheter exit-site infection and adverse reactions (including mupirocin
versus mupirocin in preventing infection secondary to tunneled,
resistance among staphylococcal isolates). Data were censored at the
time of catheter removal (when unrelated to catheter-associated infec-tion), death (when unrelated to catheter-associated infection), or theend of the study on October 4, 2004.
Materials and Methods Study Population
All adult patients who had acute or chronic renal failure and re-
Catheter-related infections were defined according to standard
quired hemodialysis via a newly inserted tunneled, cuffed central
guidelines (9,28,29). Catheter-associated bacteremia was defined as ei-
venous catheter at the Princess Alexandra Hospital between February
ther (
1 ) a single positive blood culture together with a positive culture
1, 2002, and July 28, 2004, were invited to participate in the study.
of the catheter tip or exit site with an identical organism or (
2 ) two or
Informed consent was obtained from all patients before their inclusion
more positive blood cultures (or a single positive blood culture for
S.
in the trial, and the study protocol was reviewed and approved by the
aureus ) with no evidence of infection source other than the device.
Princess Alexandra Hospital Research Ethics Committee.
Exit-site infection was defined as purulent exit-site discharge or two ofthree of the following: Exit-site erythema, tenderness, and induration
The study was a prospective, open-label, randomized, controlled
trial. Patients who were enrolled in the study were randomly as-
signed to receive either topical вР•-irradiated, commercially available,
Exit-site swabs were obtained using sterile, premoistened calcium
pooled antibacterial honeys including
Leptospermum sp honey (Medi-
alginate swabs in all suspected cases of catheter-associated infection.
honey; Medihoney Pty Ltd, Brisbane, Australia) or standard 2%
The swabs were streaked onto plates that contained blood agar, colis-
calcium mupirocin ointment (Bactroban; SmithKline Beecham Phar-
tin-nalidixic acid agar, McConkeyвАЩs media, and mannitol-salt agar. All
maceuticals, Sydney, Australia; mupirocin group) in addition to
cultures were incubated at 35°C for 48 h and examined daily for
standard exit-site care and 10% povidone iodine disinfection. The
growth. Patients with suspected bacteremia (fever ѕЊ38¬∞C, rigors, leu-
randomization was performed using sequentially numbered,
kocytosis, or clinically unwell) were investigated with exit-site swabs
opaque, sealed envelopes before catheter insertion. The sequence of
and at least two sets of blood cultures (20 ml). Staphylococcal isolates
interventions was obtained from a computer-generated random-
were screened routinely for mupirocin resistance by the disk suscepti-
number list with randomization blocks of 10.
bility method (30). The laboratory was blinded to the patientвАЩs alloca-
All patients underwent ultrasound-guided placement of a subcuta-
neously tunneled, internal jugular venous hemodialysis catheter (Perm-
In cases of suspected catheter-associated bacteremia, the catheter was
Cath; Quinton Instrument Company, Seattle, WA) by dedicated vascu-
removed and the tip was sent for microbiologic culture. Approximately
lar access surgeons according to the method described by Schwab
et al.
50 mm of catheter tip was rolled across chocolate agar plates and
(26). A prophylactic preoperative antibiotic (cephazolin 1 g intrave-
processed according to the semiquantitative method of Maki
et al. (29).
nously) was prescribed in all cases. All catheters received 10% povi-
Catheter colonization was defined as the recovery of ѕЊ15 colony-
done iodine disinfection at the site of insertion (contact time 3 to 5 min
followed by complete drying) and were covered by an opaque, air-permeable, nonwoven fabric dressing (Primapore, Smith & Nephew,
Sydney, Australia). Chest radiographs were obtained after insertion to
Normality of data was evaluated by the Kolmogorov-Smirnov test
confirm the position of the catheter tip in the superior vena cava.
with LillieforвАЩs correction. Results are expressed as mean ѕЃ SEM for
Medihoney
versus Mupirocin for Dialysis Catheters
continuous parametric data, median (interquartile range) for continu-
ysis, the type of prophylaxis administered (honey or mupiro-
ous nonparametric data, and frequencies and percentages for categor-
cin) was not significantly associated with bacteremia-free sur-
ical data. Comparisons between the honey and mupirocin groups were
vival (unadjusted hazard ratio for honey, 0.94; 95% confidence
performed using
t test or the Mann-Whitney
U test, depending on data
interval, 0.27 to 3.24;
P ѕ≠ 0.92). Multivariate analysis did not
distribution. Differences in proportions were evaluated by вРє2 or Fisher
alter this finding (data not shown). No exit-site infections were
exact test. Infection-free survival curves, survival probabilities, and
observed in any patients during the period of the study.
estimated mean survival times were generated according to theKaplan-Meier method. Differences in the survival curves between thetwo groups were evaluated using the log rank test. A multivariate
CoxвАЩs proportional hazards model was also applied, which included
Medihoney and mupirocin both were well tolerated. Tran-
allocated group, age, gender, race, body mass index, diabetic status,
sient, mild local skin discomfort was observed in one patient
ischemic heart disease, presence of infection at the time of randomiza-
who was treated with honey. This resolved within a few days
tion, nasal staphylococcal colonization, and serum albumin as covari-
despite continued administration of the agent. A similar tran-
ates. The proportional hazards assumption was checked both graphi-
sient local skin reaction associated with erythema was observed
cally and by hypothesis testing. Graphical examination was done using
in one patient who received topical mupirocin ointment. No
a log-cumulative hazard plot. The hypothesis test was carried out after
systemic adverse reactions to either honey or mupirocin oint-
generating Schoenfield and scaled Schoenfield residuals. All data were
ment were noted during the study period.
analyzed on an intention-to-treat basis using the statistical software
Mupirocin-resistant strains were not detected in any staphy-
package SPSS release version 10.0.5 (SPSS Inc., Chicago, IL).
P ѕљ 0.05
lococcal isolates from study patients with catheter-associated
Prospective power calculations for the infection-free survival analy-
bacteremias. During the period of the trial, the proportion of
ses were performed using the software package PS version 1.0.17
staphylococcal isolates from all microbiologic specimens within
(Vanderbilt University Medical Center, Nashville, TN). It was esti-
the hospital that were mupirocin resistant was 2.0% (26 of 1328
mated prospectively that the study had adequate statistical power (80%
staphylococcal isolates). Approximately 70% of these mupiro-
probability) to detect at least a doubling in mean catheter-associated
cin-resistant isolates were identified in patients from the Renal
infection-free survival from a control (mupirocin) level of 320 d if 96
Unit, but none of these individuals was involved in the present
patients were recruited in the study (48 in each group), assuming an вР£
level of 0.05, accrual time of 730 d, and additional follow-up time after
The median cost of exit-site application for the average life of
a catheter was $13.00 AUD per patient in the honey group and$11.10 AUD per patient in the mupirocin group.
Results Patient Characteristics
Discussion
A total of 101 patients required insertion of tunneled, cuffed
The present study demonstrated that regular, thrice-weekly,
central venous catheters for the provision of hemodialysis at
topical exit-site application of standardized antibacterial honey
the Princess Alexandra Hospital between June 1, 2002, and July
was safe and cost-effective and resulted in a comparable rate of
31, 2004. All agreed to participate in the study, and none was
catheter-associated infection to that obtained with topical
lost to follow-up. No patients were excluded from the study.
mupirocin exit-site application in patients with tunneled,
Fifty-one patients were randomly allocated to the honey group,
cuffed hemodialysis catheters. To our knowledge, this is the
and 50 patients received mupirocin. There were no significant
first randomized, controlled trial to have examined the poten-
differences between the two groups with respect to their base-
tial utility of honey as an antimicrobial prophylactic agent.
line characteristics, except for a higher mean age and a trend
Moreover, the results of this study are potentially generalizable
toward a greater frequency of ischemic heart disease in the
to the prevention of infections associated with a number of
mupirocin group (Table 1). Median (interquartile range) fol-
prosthetic devices (
e.g. , central venous catheters, Hickman cath-
eters, Tenckhoff catheters, T-tubes, nephrostomy tubes).
Previous randomized, controlled trials have shown convinc-
ingly that, compared with placebo or no treatment, topical
Catheter-associated bacteremias occurred with similar fre-
mupirocin application was associated with a seven- to 13-fold
quencies in honey-treated (
n ѕ≠ 6, 12%) and mupirocin-treated
reduction in catheter-associated bacteremias in patients with
patients (
n ѕ≠ 5, 10%;
P ѕ≠ 0.78). The causes of bacteremia in the
either noncuffed, nontunneled (2) or tunneled, cuffed hemodi-
honey and mupirocin groups were
S. aureus (1 or 17%
versus 1
alysis catheters (3). Moreover, the observed rates of catheter-
or 20%), coagulase-negative staphylococci (2 or 33%
versus 1 or
associated bacteremia in mupirocin-treated patients in those
20%), micrococcus (1 or 17%
versus 0 or 0%),
Serratia marcescens
studies (0.7 and 1.6 episodes per 1000 catheter days, respec-
(2 or 33%
versus 0 or 0%),
Klebsiella pneumoniae (0 or 0%
versus
tively) were similar to those observed in the present investiga-
1 or 20%), and
Stenotrophomonas maltophilia (0 or 0%
versus 2 or
tion (0.85 episodes per 1000 catheter-days). However, since the
40%). The incidences of bacteremia in the two groups were 0.97
publication of these earlier investigations, there has been in-
and 0.85 episodes per 1000 catheter-days, respectively (NS).
creasing concern regarding the emergence of mupirocin-resis-
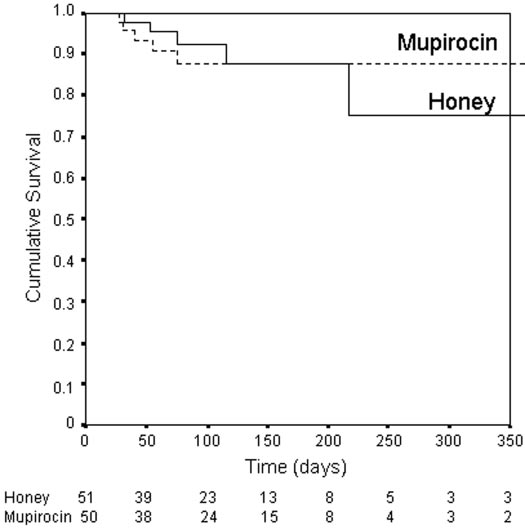
Mean ѕЃ SE actuarial bacteremia-free survival periods were
tant staphylococci (31) and the potential for therapeutic failure
367 ѕЃ 42 and 334 ѕЃ 17 d, respectively (log rank 0.01,
P ѕ≠ 0.92;
(15). After introducing mupirocin chemoprophylaxis in our
Figure 1). On univariate Cox proportional hazards model anal-
own unit for the prevention of peritoneal dialysis and hemodi-
Journal of the American Society of Nephrology
Table 1. Baseline patient characteristics
alysis catheter infections, high-level mupirocin resistance has
Continued use of topical antimicrobial agents has provided
emerged, ranging between 2 and 6% of all staphylococcal iso-
the selective pressure that has led to the emergence of antibi-
lates. None of the isolates from patients in the present study
otic-resistant strains, which, in turn, has driven the continued
displayed mupirocin resistance, although this may have been
search for alternative, safer topical antiseptic agents with
due to the relatively small patient numbers and short duration
broad-spectrum antimicrobial activities. In this regard, stan-
of follow-up. Another group (32) has not observed an increase
dardized antibacterial honey seems to be a very promising
in high-level resistance after topical mupirocin administration,
candidate. Although mupirocin has been shown to be effective
but this finding is contradicted by several reports of disturbing
primarily against Gram-positive organisms, selected honeys
increases in resistance (to between 12.4 and 66% of staphylo-
have been found to be highly effective against fungi (including
coccal isolates) (31,33вАУ35), particularly with widespread and
Aspergillus fumigatus ,
Aspergillus flavus ,
Penicillium citrinum ,
prolonged mupirocin use (31). Furthermore, Perez-Fontan
et al.
Trichophyton rubrum ,
Trichophyton tonsurans , and
Candida albi-
(34) observed a greater incidence of exit-site infections in pa-
cans ), Gram-negative bacteria (including
Escherichia coli ,
Kleb-
tients who were colonized with mupirocin-resistant
S. aureus
siella pneumoniae ,
Pseudomonas spp. ,
Proteus mirabilus ,
Haemophi-
compared with those who were colonized with sensitive organ-
lus influenzae ,
Enterobacter cloacae , and
Shigella dysenteriae ), and
isms, suggesting that the development of mupirocin resistance
Gram-positive organisms (including streptococci, staphylo-
can have adverse clinical consequences.
cocci, enterococci, and clostridia) (18,22). The minimum inhib-
Medihoney
versus Mupirocin for Dialysis Catheters
occasionally been reported to contain viable spores of
Clostrid-ium botulinum (41).
The potential weaknesses of this trial were its open-label
design, the possibility of type 2 statistical error, and the lack ofstatistical power to confirm therapeutic equivalence of honeyand mupirocin. The absence of blinding could have potentiallyintroduced co-intervention and observer biases. For example,Wagman
et al. (42) showed an eightfold higher rate of infectionsassociated with tunneled, cuffed catheters that were managedoutside study protocol compared with those that were man-aged using the technique required by the study. Such protocoldeviations were strictly avoided in the present study by ensur-ing that nursing staff adhered to a standardized exit-site careprotocol and carefully documented their actions at each dress-ing change. Moreover, observer bias was minimized by the useof clearly defined, objective outcome measures and by blindingto the patientвАЩs study group assignment the microbiology lab-oratory staff who processed culture samples. As stated in theMaterials and Methods section, the study was adequately pow-ered to have detected a halving (or doubling) of risk in thehoney arm compared with the mupirocin arm. A smaller sig-nificant difference between the two groups could not be ex-
Figure 1. Catheter-associated bacteremia-free survival in honey-
cluded because of the possibility of a type 2 statistical error. In
and mupirocin-treated patients. The difference between the
particular, it is important to emphasize that the study lacked
groups was not statistically significant (log rank score 0.33,
P ѕ≠
statistical power to have determined confidently that honey
0.87). The number of patients at risk within each group is
and mupirocin were therapeutically equivalent. Although the
indicated beneath the corresponding time periods on the
x axis.
limits for establishing equivalence are arbitrary, to have had an80% probability of determining that the differences betweenhoney and mupirocin were no greater than 10% using the as-
itory concentrations of honey for all of these species were
sumptions of the original power calculations, a minimum of 4688
generally well below 10% vol/vol (18,22,24,36) and did not
patients in total would have been required. The results of the
seem to be appreciably different in antibiotic-resistant strains,
present trial therefore should be considered preliminary, such that
such as methicillin-resistant
S. aureus , multidrug-resistant
much larger studies will be needed to confirm that honey offers
Gram-negative organisms, and vancomycin-resistant entero-
prophylactic efficacy that is equivalent to mupirocin.
cocci (18,24). The lack of significant variance in the sensitivity to
In conclusion, the present investigation demonstrated that
some honeys of a large number of isolates collected from a wide
the application of honey (Medihoney) to the exit sites of tun-
range of clinical settings contrasts markedly with the variations
neled, cuffed hemodialysis catheters was safe and effective
seen in antimicrobial sensitivities to antibiotics and strongly
compared with topical 2% calcium mupirocin, although our
suggests that there is no mechanism of resistance to the anti-
investigation did not have sufficient statistical power to con-
bacterial activity of honey (37). Indeed, despite a considerable
firm therapeutic equivalence. This study has potentially impor-
accumulated experience of honey use in wound infections,
tant implications for the treatment of hemodialysis patients
antimicrobial resistance has not yet been reported.
with temporary hemodialysis catheters and possibly for the
The mechanisms of action of honey have not been fully
treatment of patients with other types of catheters and pros-
elucidated, but hyperosmolality, acidity, hydrogen peroxide
thetic devices, who are at greatly increased risk for morbidity
generation, and phytochemical components (including fla-
and mortality from catheter-related sepsis. The finding that
vonoids and phenolic acids) have been considered to be impor-
honey administration to such patients is safe, inexpensive, un-
tant (17,36). The floral source of the honey also seems to be
likely to select for further antibiotic-resistant strains, and asso-
crucial, because some honeys (
e.g. , manuka honey from New
ciated with acceptably low catheter-related bacteremia rates
Zealand and a related
Leptospermum honey from Australia) can
suggests that this agent may represent a satisfactory, alternative
be up to 100 times more active against microorganisms than
means of preventing hemodialysis catheter infections. Future
others (36). Honey has also been demonstrated to possess a
much larger trials are recommended to confirm the equivalence
number of additional advantages over conventional topical
of honey and mupirocin chemoprophylaxis.
antiseptics, including the promotion of wound healing (22),activation of lymphocytes and neutrophils (38), and the lack of
Acknowledgments
significant toxicity to human tissues (39). Sterilization of honey
The invaluable assistance of the nursing staff of the Princess Alex-
by вР•-irradiation does not cause loss of antimicrobial activity
andra Hospital Hemodialysis Unit is gratefully acknowledged. The
(40) but is recommended before clinical use because honey has
honey used in this trial was provided by Medihoney Pty Ltd.
Journal of the American Society of Nephrology
Contributors: Protocol development: D.W. Johnson, C.M. Hawley,
14. Keohane PP, Jones BJ, Attrill H, Cribb A, Northover J, Frost
S.B. Campbell, N.M. Isbel, G.R. Nimmo, and H. Gibbs; patient recruit-
P, Silk DB: Effect of catheter tunnelling and a nutrition
ment and management: D.W. Johnson, C. van Eps, D.W. Mudge, K.J.
nurse on catheter sepsis during parenteral nutrition. A
Wiggins, K. Armstrong, C.M. Hawley, S.B. Campbell, and N.M. Isbel;
controlled trial.
Lancet 2: 1388 вАУ1390, 1983
microbiologic studies: G.R. Nimmo; data analysis: D.W. Johnson, C.
15. Cookson BD, Lacey RW, Noble WC, Reeves DS, Wise R,
van Eps, D.W. Mudge, K.J. Wiggins, K. Armstrong, C.M. Hawley, S.B.
Redhead RJ: Mupirocin-resistant
Staphylococcus aureus .
Campbell, N.M. Isbel, G.R. Nimmo, and H. Gibbs; manuscript prepa-
ration: D.W. Johnson, C. van Eps, D.W. Mudge, K.J. Wiggins, K. Arm-
16. Zumla A, Lulat A: HoneyвАФA remedy rediscovered.
J R Soc
strong, C.M. Hawley, S.B. Campbell, N.M. Isbel, G.R. Nimmo, and H.
17. Namias N: Honey in the management of infections.
Surg
Infect (Larchmt) 4: 219 вАУ226, 2003
18. Efem SE, Udoh KT, Iwara CI: The antimicrobial spectrum
References
of honey and its clinical significance.
Infection 20: 227вАУ229,
1. Marr KA, Sexton DJ, Conlon PJ, Corey GR, Schwab SJ,
Kirkland KB: Catheter-related bacteremia and outcome of
19. Subrahmanyam M: Early tangential excision and skin
attempted catheter salvage in patients undergoing hemo-
grafting of moderate burns is superior to honey dressing:
dialysis.
Ann Intern Med 127: 275вАУ280, 1997
A prospective randomised trial.
Burns 25: 729 вАУ731, 1999
2. Sesso R, Barbosa D, Leme IL, Sader H, Canziani ME, Man-
20. Molan PC: Potential of honey in the treatment of wounds
fredi S, Draibe S, Pignatari AC:
Staphylococcus aureus pro-
and burns.
Am J Clin Dermatol 2: 13вАУ19, 2001
phylaxis in hemodialysis patients using central venous
21. Dunford C, Cooper R, Molan P: Using honey as a dressing
catheter: Effect of mupirocin ointment.
J Am Soc Nephrol 9:
for infected skin lesions.
Nurs Times 96: 7вАУ9, 2000
22. Moore OA, Smith LA, Campbell F, Seers K, McQuay HJ,
3. Johnson DW, MacGinley R, Kay TD, Hawley CM, Camp-
Moore RA: Systematic review of the use of honey as a
bell SB, Isbel NM, Hollett P: A randomized, controlled trial
wound dressing.
BMC Complement Altern Med 1: 2, 2001
of topical exit site mupirocin application in patients with
23. Cooper RA, Halas E, Molan PC: The efficacy of honey in
tunnelled, cuffed haemodialysis catheters.
Nephrol Dial
inhibiting strains of
Pseudomonas aeruginosa from infected
burns.
J Burn Care Rehabil 23: 366 вАУ370, 2002
4. Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG: Vas-
24. Cooper RA, Molan PC, Harding KG: The sensitivity to
cular access and all-cause mortality: A propensity score
honey of Gram-positive cocci of clinical significance iso-
analysis.
J Am Soc Nephrol 15: 477вАУ 486, 2004
lated from wounds.
J Appl Microbiol 93: 857вАУ 863, 2002
5. USRDS: Excerpts from the USRDS 2002 annual data report:
25. Dixon B: Bacteria canвАЩt resist honey.
Lancet Infect Dis 3: 116,
Atlas of end-stage renal disease in the United States.
Am J
26. Schwab SJ, Buller GL, McCann RL, Bollinger RR, Stickel
6. Pisoni RL: Vascular access use and outcomes: Results from
DL: Prospective evaluation of a Dacron cuffed hemodial-
the DOPPS.
Contrib Nephrol 13вАУ19, 2002
ysis catheter for prolonged use.
Am J Kidney Dis 11: 166 вАУ
7. Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF,
Port FK: Type of vascular access and mortality in U.S.
27. National Kidney Foundation: K/DOQI clinical practice
hemodialysis patients.
Kidney Int 60: 1443вАУ1451, 2001
guidelines for vascular access, 2000.
Am J Kidney Dis 37:
8. Pastan S, Soucie JM, McClellan WM: Vascular access and
increased risk of death among hemodialysis patients.
Kid-
28. Division of Nosocomial and Occupational Infectious Dis-
9. Randolph AG, Cook DJ, Gonzales CA, Brun-Buisson C:
eases, Bureau of Infectious Diseases, Laboratory Centre for
Tunneling short-term central venous catheters to prevent
Disease Control, Health Canada: Preventing infections as-
catheter-related infection: A meta-analysis of randomized,
sociated with indwelling intravascular access devices.
Can
controlled trials.
Crit Care Med 26: 1452вАУ1457, 1998
Commun Dis Rep 23[Suppl 8]: i-iii, 1вАУ32, i-iv, 1вАУ16, 1997
10. Flowers RH, Schwenzer KJ, Kopel RF, Fisch MJ, Tucker SI,
29. Maki DG, Weise CE, Sarafin HW: A semiquantitative cul-
Farr BM: Efficacy of an attachable subcutaneous cuff for
ture method for identifying intravenous-catheter-related
the prevention of intravascular catheter-related infection.
infection.
N Engl J Med 296: 1305вАУ1309, 1977
A randomized, controlled trial.
JAMA 261: 878 вАУ 883, 1989
30. Finlay JE, Miller LA, Poupard JA: Interpretive criteria for
11. Maki DG, Stolz SM, Wheeler S, Mermel LA: Prevention of
testing susceptibility of staphylococci to mupirocin.
Anti-
central venous catheter-related bloodstream infection by
microb Agents Chemother 41: 1137вАУ1139, 1997
use of an antiseptic-impregnated catheter. A randomized,
31. Conly JM, Vas S: Increasing mupirocin resistance of
Staph-
controlled trial.
Ann Intern Med 127: 257вАУ266, 1997
ylococcus aureus in CAPDвАФShould it continue to be used as
12. Timsit JF, Sebille V, Farkas JC, Misset B, Martin JB, Chevret
prophylaxis?
Perit Dial Int 22: 649 вАУ 652, 2002
S, Carlet J: Effect of subcutaneous tunneling on internal
32. Lobbedez T, Gardam M, Dedier H, Burdzy D, Chu M, Izatt
jugular catheter-related sepsis in critically ill patients: A
S, Bargman JM, Jassal SV, Vas S, Brunton J, Oreopoulos
prospective randomized multicenter study.
JAMA 276:
DG: Routine use of mupirocin at the peritoneal catheter
exit site and mupirocin resistance: Still low after 7 years.
13. de Cicco M, Panarello G, Chiaradia V, Fracasso A, Veronesi
Nephrol Dial Transplant 19: 3140 вАУ3143, 2004
A, Testa V, Santini G, Tesio F: Source and route of micro-
33. Annigeri R, Conly J, Vas S, Dedier H, Prakashan KP, Barg-
bial colonisation of parenteral nutrition catheters.
Lancet 2:
man JM, Jassal V, Oreopoulos D: Emergence of mupirocin-
resistant
Staphylococcus aureus in chronic peritoneal dialysis
Medihoney
versus Mupirocin for Dialysis Catheters
patients using mupirocin prophylaxis to prevent exit-site
37. Cooper RA, Molan PC, Harding KG: Antibacterial activity
infection.
Perit Dial Int 21: 554 вАУ559, 2001
of honey against strains of
Staphylococcus aureus from in-
34. Perez-Fontan M, Rosales M, Rodriguez-Carmona A, Falcon
fected wounds.
J R Soc Med 92: 283вАУ285, 1999
TG, Valdes F: Mupirocin resistance after long-term use for
38. Tonks AJ, Cooper RA, Jones KP, Blair S, Parton J, Tonks A:
Staphylococcus aureus colonization in patients undergoing
Honey stimulates inflammatory cytokine production from
chronic peritoneal dialysis.
Am J Kidney Dis 39: 337вАУ341,
monocytes.
Cytokine 21: 242вАУ247, 2003
39. Molan PC: A brief review of the use of the use of honey as
35. Cavdar C, Atay T, Zeybel M, Celik A, Ozder A, Yildiz S,
a clinical dressing.
Aust J Wound Manag 6: 148 вАУ158, 1998
Gulay Z, Camsari T: Emergence of resistance in staphylo-
40. Molan PC, Allen KL: The effect of gamma-irradiation on
cocci after long-term mupirocin application in patients on
the antibacterial activity of honey.
J Pharm Pharmacol 48:
continuous ambulatory peritoneal dialysis.
Adv Perit Dial
41. Mossel DA: Honey for necrotic breast ulcers.
Lancet 2: 1091,
36. Willix DJ, Molan PC, Harfoot CG: A comparison of the
sensitivity of wound-infecting species of bacteria to the
42. Wagman LD, Kirkemo A, Johnston MR: Venous access: A
antibacterial activity of manuka honey and other honey.
prospective, randomized study of the Hickman catheter.
J Appl Bacteriol 73: 388 вАУ394, 1992
Source: http://www.woundviewer.med-surv.de/downloads/public/johnson-medihoney-paper-JASN-2005.pdf
Glossar Kokainbehandlungen √Ьbersicht √Љber den Stand der Behandlungen von kokainbedingten St√ґrungen Rudolf Stohler, Dr. med., Psychiatrische Universit√§tsklinik Z√Љrich Toni Berthel, Dr. med., Integrierte Psychiatrie Winterthur Michael Herzig, Ambulante Drogenhilfe/Heroingest√Љtzte Behandlung der Stadt Z√Љrich Peter Burkhard, Die ALTERNATIVE, Ottenbach Thomas Meyer, Dr. me
GenScript Adenoviral Vector-based siRNA Protocol Technical Manual No. 0165 Version 04032007 Introduction вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶. Vector-based siRNA вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶ Adenoviral siRNA Vector вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶вА¶в
A |
B |
C |
D |
E |
F |
G |
H |
I |
J |
K |
L |
M |
N |
O |
P |
Q |
R |
S |
T |
U |
V |
W |
X |
Y |
Z |
0-9 |
 Medihoney versus Mupirocin for Dialysis Catheters
occasionally been reported to contain viable spores of Clostrid-ium botulinum (41).
Medihoney versus Mupirocin for Dialysis Catheters
occasionally been reported to contain viable spores of Clostrid-ium botulinum (41).